Ce site est disponible en Français ou en Anglais. Pour changer de langue, cliquer sur le drapeau correspondant.
This site is available in English or French language. To change the language, click on the corresponding flag.
Last updated: January 12, 2019 Dernière mise à jour: 12 Janvier 2019
BIENVENUE sur ce site dédié à la physiologie de la mastication et la déglutition et à ses conséquences cliniques. Les données développées ici sont le résumé d’un travail commencé il y a plus de 30 ans avec Jean-François Lauret (†2005). Elles ont permis de mieux comprendre les fondements et le fonctionnement réel de notre appareil manducateur lors de la mastication et la déglutition. Les différences fondamentales qui vont progressivement apparaître, avec les concepts occlusaux gnathologiques enseignés comme des dogmes et remontant pour certains à presque un siècle, montrent qu’un changement de paradigme ne pourra pas être évité. Bonne lecture. Dr Marcel Le Gall

WELCOME on this website dedicated to mastication and deglutition physiology and their clinical consequences. The data developed below, are the summary of a work begun more than 30 years ago with Jean-François Lauret (†2005). They have allowed, to best understand the basis and the real functioning of the human masticatiory tract during chewing function and swallowing. Fundamental differences, will progressively appear, with the Gnathologic occlusal concept, always taught as a dogma and dating from almost one century for a share, show that, a change of the paradigm is became necessary. Good reading ! Dr Marcel Le Gall
Les vidéos ont une importance primordiale pour comprendre la cinétique des cycles de mastication et ses relations avec le guidage occlusal des dents postérieures. Elles peuvent être revues plusieurs fois si nécessaire et observées image par image. NOTER qu’en faisant un double clic sur les vidéos, elles apparaîtront en plein écran.
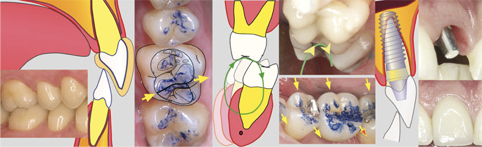
Fig A1: Vidéo clinique de mastication chez un homme de 28 ans présentant des guidages optimaux en occlusion de classe 1. Noter l’orientation centripète des cycles et les guidages équilibrés sur toute l’étendue des faces occlusales des dents postérieures, du côté mastiquant.
Movies are of premium importance for understand the kinetics of mastication, accorded with occlusal guidance.They may be revised several times if necessary and observed frame by frame. If a double click is done on the videos, they will appear in full screen.
Fig A1: Movie of chewing function in a 28 years old man, with optimal occlusal guidance. Note the centripetal direction of the cycles, and the guidances balanced on the whole extent of the occlusal surfaces of posterior teeth.
Bibliographie
- N’Gom P, Bonnet L, Woda A. “Influence de la mastication sur la santé” Info. Dent. 2000; 19 (10 Mai): 1367-1378